Here at 10to8 we love data — but are statistics the final piece in the puzzle of patient...
Ten Top Ways to Withstand Winter Pressure in your GP Surgery
It’s that time of year again – winter is coming! And while it brings with it a flurry of festivities, lights, decorations, delicious foods, and general merriment, winter can also bring an abundance of problems in its wake. One of these problems is the significant effect winter pressure has on medical practices.
Many practice owners will already be preparing for the onslaught of colds, flu, and other winter ailments. This year, in particular, is likely to be increasingly tough as the seasonal flu vaccinations collide with COVID-19 booster shots, meaning practices need to schedule more appointments, see more patients, and overall have more work to do to survive the season.
Winter can also make workplaces more hazardous for employees. Working conditions such as cold temperatures, poor indoor air quality, low lighting, and risk of physical hazards (such as icy commutes) all need to be thought about. This, coupled with the general winter blues, means it’s no wonder that winter is a stressful time for medical staff.
However, there are ways to make it through the storm. We’ve taken a look at some of the ways that medical practices can alleviate some of the pressure on their shoulders in winter and stay afloat. Here are the top 10 ways to withstand winter pressure in your GP surgery.
How does winter pressure affect medical practices?
First of all, let’s take a look at all the ways in which winter pressure can affect the healthcare industry.
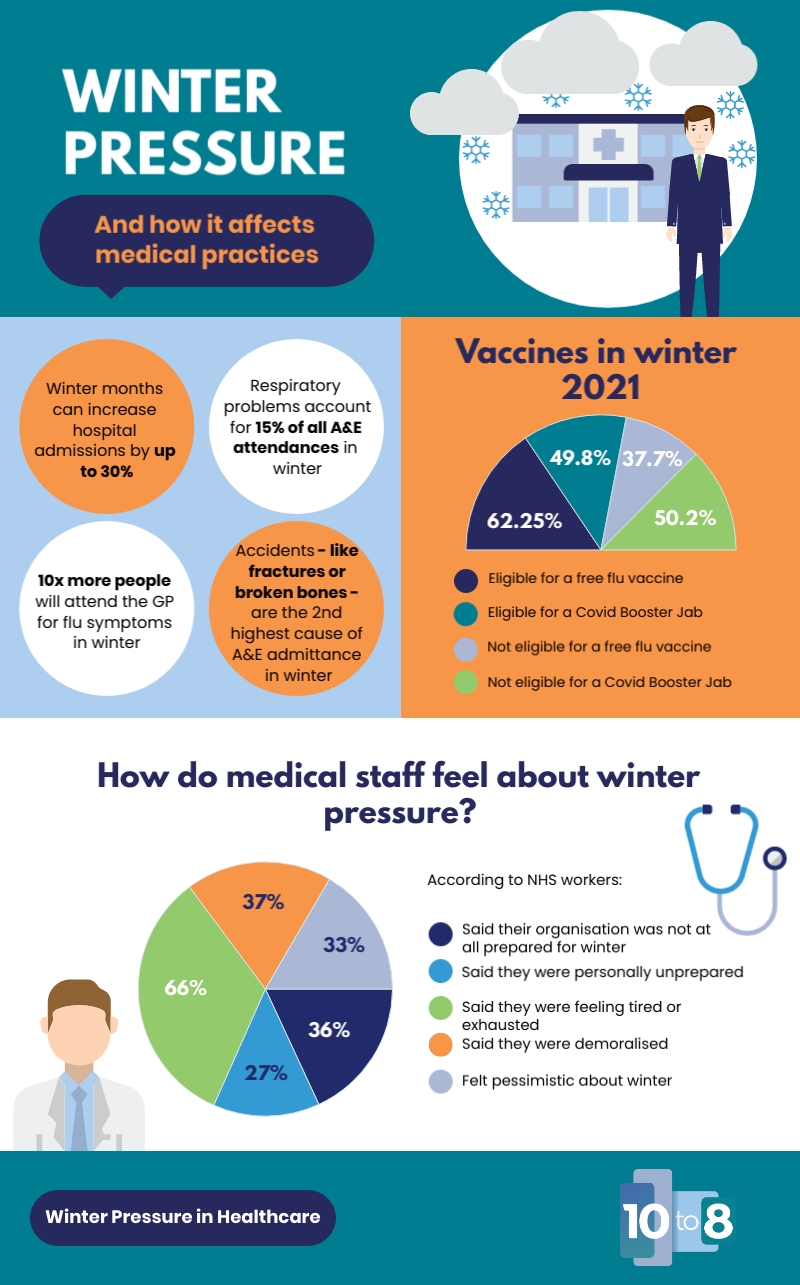
The winter months cause an increase in hospital admissions of up to 30%. This significant increase has a wide-reaching impact on medical practices. For example, along with spending more time with patients, doctors may also have to work longer hours during winter compared to summer.
Many patients with respiratory problems experience worsened conditions or develop infections during the winter months and need to be seen urgently. In fact, respiratory problems generally account for 15% of all A&E attendances in winter. This is particularly brutal with the elderly, as higher mortality rates are seen in people 75 or older.
In addition, winter weather causes accidents – such as slipping on black ice or hazards from driving in bad weather conditions. Accidents are the second-highest cause of A&E admittance in winter is due to fractures, broken bones, and other injuries which often require urgent care. The higher demand for services can put a strain on a GP practice’s resources – from staff members to equipment.
It is important that medical practices prepare for the winter months, and have a plan in case they are overwhelmed with patients. Getting organized beforehand can help your practice be prepared to manage this increase of patient visits successfully!
How does the flu contribute to winter pressure in healthcare?
The flu can have a detrimental impact on those working in healthcare. Outbreaks of the illness are much more common in winter. Plus, the strain of flu can vary year on year, causing variation in how badly people are affected and who is affected the worst.
Outbreaks of flu can also zap up the medical industry’s resources. As more and more ambulances are called to tend to flu patients, the emergency phone line and primary care services are put under added stress. But the majority of people will go to a GP for their flu-like symptoms as opposed to calling the emergency services. In fact, around 10 times more people will attend the GP for flu symptoms during the winter, meaning that practices will have to find a way to cope with the added demand.
What about the flu vaccination?
The flu vaccination certainly helps lessen the impact of some of these problems. However, it doesn’t rid the world of flu itself and creates a few new issues for GP practices.

This year many governments, including the UK, are launching the biggest flu vaccination program they’ve ever done, in an attempt to combat the increasing rate of influenza-like infections across the world.
More than 35 million people in England – that’s over half of the entire population – are eligible for a free flu vaccine. On top of this, 28 million people are eligible for their COVID-19 booster jabs. The sheer number of appointments that need to be booked in to handle this is quite incredulous, and many practices around the country don’t have the assistance of a medical booking system to allow patients to book their own slots.
As a result, it’s not just doctors and nurses that will feel the pressure, but admin teams will also be working overtime. They are one of the unsung heroes in a GP practice, but their contribution is pivotal to ensuring that vaccines are successfully administered and medical practices stay afloat during the winter months.
How do medical staff cope with winter pressure?
A recent survey of medical workers showed that 36% said their organization was not at all prepared for winter. Many workers are feeling overworked with 27% reporting they feel tired. And with the general vibe of demoralization and pessimism, it is no surprise that many are feeling burned out at work.
But with an increase in demand comes an increase in the need to prepare. So, let’s take a look at how to survive winter pressure in the medical industry and stay afloat during these busy months.
How to cope with winter pressure in healthcare
Get an efficient appointment booking system
Scheduling medical appointments can take up a significant portion of the day for practices. Admin staff have to be constantly on the ball, answering phone calls and dealing with inquiries, and, for patients, sitting on hold to the doctor can seem like a long process. If you are looking at ways to increase medical productivity, it’s time for an efficient appointment booking system.
Medical scheduling systems, like 10to8, can solve a lot of complications with winter bookings. Not only can they make bookings more efficient for patients, but also transform the entire booking process, save countless admin hours (meaning staff can be delegated elsewhere), reduce DNAs, and even offer accessible appointment scheduling for those with disabilities. In the winter months, you could also consider:
- Planning to provide more telephone or virtual appointments to remote patients or those less willing to travel in the icy weather
- For most medicines, repeat drug requests could be extended to 90 days.
- Suspending certain appointment types to free up time to treat those in need. This could include coil fittings, new routine referrals, or even minor surgeries.
- Limiting surgeries to emergencies only
All these types of changes to the way your practice handles appointments can have a significant effect on how your practice is managed overall in the winter.
Implement online tools
These days, there are so many different pieces of software and virtual tools available for doctors and practice owners. From allowing patients to order their own prescriptions to reducing patient no-shows, using virtual tools can seriously help reduce some winter pressure for GP practices.
Medical software can also help integrate various aspects of a medical business together. For instance, emailing invoices from the practice management system, having customers book their own appointments online, or storing patient details in a way that can be accessed anywhere by anyone with an internet connection.
Make a business continuity, emergency, and recovery plan
In case of emergency, it is important that every practice has a plan in place – this needs to be a plan that everyone knows and follows. Practice owners and staff should know the exact protocol for what they would do if there was a flu outbreak for instance. Or what would happen if there was a weather-related emergency that affected the surgery. In fact, all across the country, medical practices should stay informed of both national and local cold-weather resilience plans.
These sorts of plans are created to get the service back up and running as soon as possible if issues arise. This could be things like providing remote care to patients or ensuring the practice has a supply of emergency equipment, or even simply getting computers back up and running. But, it should always focus on the most critical aspect of care first.
Before the cold weather hits, these procedures should be reviewed to ensure that you’re adequately prepared for winter.
Prepare as much as possible
In winter, the key is preparation. Practice owners should ensure that they have thought about every eventuality and covered all possible things that could go wrong.
A couple of ways you can do this are to evaluate some of the day-to-day things you do that don’t actually involve speaking to patients. Preparing prescriptions, filing documents, and administrative tasks that require the use of a computer may all be examples.
Think about how can these be arranged in such a way that the most pressing issues are prioritized. For example, how would they be handled if there is a major flu outbreak or staff members are absent? You may also need to consider teaching senior administrative staff how to follow a process for prioritizing admin work and ensuring that critical paperwork is dealt with efficiently.
Brace yourself for the cold
This may sound inevitable, but it is important to prepare your practice for winter weather. If you have a heating system in place, make sure it’s working – and if not, get a new one! Ensure your boiler is well-maintained, and that if there are any issues with the system when it gets cold, you, and your staff, should know exactly who to call.
It is also recommended that a supply of safe emergency lighting, including flashlights with batteries, be maintained. In addition, check outside your practice or surgery to ensure that there aren’t any trees or branches which might cause damage during bad weather. Ensure paths and car parks are gritted and that you have an emergency supply of grit in case the roads get really bad.
Also, have a supply of warm clothes and blankets on hand in case you do lose power or heating – it might be good to keep some spares at the office just in case!
Lastly, it might be wise to encourage staff to work from home where possible, especially in particularly icy conditions. Avoiding unnecessary travel can go a long way to keeping your staff members safe.

But, for those who do have to go out on the road, make sure they have high visibility clothing, spare warm clothing or blankets, and a mobile phone to reach out for help.
Promote self-care
Winter is the height of flu season so, naturally, lots of people will be coming to the surgery with ailments like coughs, sniffles, and the common cold. However, in many cases, these can be treated from home with over-the-counter remedies, and patients don’t have to come into the surgery unless they are really unwell.
This can seriously help alleviate some of the pressure that practices feel during wintertime and has the added benefit that patients can be treated in their own homes where they feel most comfortable rather than traveling to the surgery.
Practitioners can encourage this by sending emails or pamphlets to patients with useful information on how to recognize the flu, how to treat coughs and colds, and when to seek medical assistance.
Also, encourage people to take their flu jabs. This can be a vital step to preventing the spread of infection and disease, and even saving lives and practices should ensure that as many eligible people as possible are vaccinated.
Make time for your own health
As well as encouraging your patients to look after themselves, it’s also important to take some time for your own health, as a GP owner, or medical staff member. Winter is a tough time of year – it’s bleak, cold, and dark outside, which means that people are inclined to spend less time outdoors.
This lack of sunlight, coupled with increased business at the practice, can contribute to increased stress and depression levels. It’s important that practice owners make time for self-care during this season, or else risk also burning out themselves.
Make people aware of infection control
Another reason for taking care of both yourself and your patients is, in the event of a severe flu outbreak, controlling infection transmission in the practice is critical. Staying at home, instead of coming to the doctor’s surgery, can really help to prevent the spread.
It is also really important that your patients are aware of the need to maintain good hygiene. Ensure everyone who comes to the surgery, patients and staff members alike, is aware of how they should be washing their hands and covering their mouths when coughing or sneezing.
To further help prevent flu outbreaks and spread, you could also.
- Have a separate waiting area for flu patients to prevent contamination to other patients
- Have sanitation stations around your GP practice to help people keep clean
- Provide staff treating flu patients additional PPE and ensure there is enough of this ordered to cover the winter season
- You could even consider having doctors that specifically treat flu patients to minimize the risk of infection spread
Implementing changes like this can help reduce infection spread which, in turn, can help reduce a lot of the effects of winter pressure.
Think ahead for vulnerable patients
Every practice should also have procedures in place to protect those who are most vulnerable from the harshness of the winter months. This could include:
- Sending out a letter to patients who are especially vulnerable during the cold months. This could include those with respiratory conditions like asthma, people over 65 years of age, pregnant women, and children under 12 months old.
- Make sure that you have emergency supplies of medications on hand, such as insulin, just in case.
- Having a team of staff members who are dedicated to making sure vulnerable patients stay safe during winter weather can be incredibly beneficial.
- Teaming up with other organizations to help the vulnerable, for instance, social services, care homes, hospitals, or community groups.
If such staff find a vulnerable patient living in poor conditions, they should be encouraged to take action. This could include providing services to help keep the patient warm, advising patients and carers about how to seek help to keep warm, or even supporting them with purchasing winter clothing or working to help resolve heating issues.
Overall…
GP practices need to be proactive in order to tackle winter pressure in their practice. GP’s should have a plan, and if they don’t have one yet, it is time for them to get started. This will not only make sure that your patient care remains high quality, but it will also allow you to effectively protect both patients and staff from an illness during these cold months ahead.





Blog comments